Article: Evidence for Efficacy of New Hsp90 Inhibitors Revealed by Ex Vivo Culture of Human Prostate Tumors
Clinical Cancer Research 2012 Jul 1;18(13):3562-70.
doi: 10.1158/1078-0432.CCR-12-0782. Epub 2012 May 9.
https://clincancerres.aacrjournals.org/content/18/13/3562.long
Authors:
Margaret M. Centenera1, Joanna L. Gillis1, Adrienne R. Hanson1, Shalini Jindal1, Renea A. Taylor3, Gail P. Risbridger3, Peter D. Sutherland2, Howard I. Scher4, Ganesh V. Raj5, Karen E. Knudsen6, Trina Yeadon for the Australian Prostate Cancer BioResource1, Wayne D. Tilley1, and Lisa M. Butler1
Affiliations:
1 Dame Roma Mitchell Cancer Research Laboratories and Adelaide Prostate Cancer Research Centre, University of Adelaide and Hanson Institute, Adelaide;
2 Urology Unit, Surgical Specialties Service, Royal Adelaide Hospital, Adelaide;
3 Prostate and Breast Cancer Research Group, Department of Anatomy and Developmental Biology, Monash University, Clayton, Australia;
4 Genitourinary Oncology Service, Memorial Sloan-Kettering Cancer Center, New York;
5 Department of Urology, UT Southwestern Medical Center at Dallas, Dallas, Texas; and
6 Kimmel Cancer Center, Thomas Jefferson University, Philadelphia, Pennsylvania
Funders:
This research received funding from the Prostate Cancer Foundation of Australia/Cancer Australia (ID 627229 to L.M. Butler, W.D. Tilley, and H.I. Scher), the Royal Adelaide Hospital Research Committee (to L.M. Butler and M.M. Centenera), the National Health and Medical Research Council of Australia (ID 627185 to W.D. Tilley, L.M. Butler and H.I. Scher). The Adelaide Prostate Cancer Research Centre is supported by an establishment grant from the Prostate Cancer Foundation of Australia (ID 2011/0452). The Australian Prostate Cancer BioResource is supported by the National Health and Medical Research Council of Australia (enabling grants 290456 and 614296) and Prostate Cancer Foundation of Australia.
Terminology:
Inhibitors (as a pharmaceutical agent/drug): Bind to a molecule to reduce its activity and affect a biological pathway.
Hsp90 protein: A chaperone protein which has important roles in cellular processes. It helps other proteins take shape, protect against stress and aids cell death.
Prostate cancer: The uncontrolled growth of cells in the prostate which is a gland in the male reproductive system.
Tumour: A collection of cell growth that may be benign or malignant (cancerous).
Potency (of a drug): The amount of drug needed to produce a given effect.
Aim:
The Hsp90 protein helps prostate tumours grow by stabilising other proteins. Compared to non-cancerous cells, prostate cancer cells are richer in this Hsp90 protein.
Disrupting prostate tumour growth could be achieved through blocking this Hsp90 protein.
Unfortunately, early drug trials acting to curb Hsp90 (such as 17-AAG) have not been very effective.
Two other Hsp90 inhibitors, AUY922 and HSP990, have shown potential to block Hsp90. This study aims to investigate these two drugs and how they compare to 17-AAG in human prostate cancer cell lines (in vitro) and primary prostate tumours (ex vivo).
Method:
In vitro
Human prostate carcinoma cells (LNCaP, VCaP and PC-3) were treated with a vehicle control or three inhibitors of Hsp90: 17-AAG, HSP990 or AUY922. Cell lines were acquired from the American Type Culture Collection. Trypan blue dye exclusion was used to test for cell growth and death under the influence of these inhibitors. Treated cell lines also underwent flow cytometric analysis to understand how these drugs may affect different stages of the cell life cycle. Likewise, DAPI staining was used to show DNA changes in cells.
Ex vivo
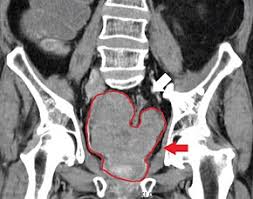
Prostate tumours were dissected and cultured with AUY922, HSP990 or 17-AAG. These tumours were obtained with consent from men who underwent a radical prostatectomy at the Royal Adelaide Hospital.
Prostate tissue was broken up (lysed) and cellular proteins studied with immunoblotting. This technique involves using specific antibodies that stick to proteins of interest.
Tissue slides also underwent immunohistochemical staining, were photographed and inspected under a microscope. Ki67 and cleaved caspase 3+ve nuclei percentages were estimated by counting cancerous cells. Ki67 was used as a protein marker of cancer and cleaved caspase 3 as a sign of cell death (the opposite of tumour growth).
Results:
In vitro
AUY922 and HSP990 were more potent than 17-AAG in prostate cancer cells. In cell lines treated with AUY922 and HSP990 compared to 17-AAG:
- Cell growth was stopped more effectively
- Cell death was stimulated more
- Cells were arrested in the G2-M phase of the cell cycle and pushed towards cell death (PC-3 and LNCaP cell lines)
- DNA chromatin was more condensed
- Cell death was observed visually with features such as membrane blebbing
- Hsp90 inhibition was detected by elevated Hsp70 and reduced markers (PC-3 and LNCaP cell lines)
Ex vivo
Hsp70 was higher in tumours cultured with 17-AAG, AUY922 or HSP990 which shows inhibition of Hsp90. Only AUY922 and HSP990 trigged significant cell death and growth prevention (anti-tumour).
Conclusion:
Synthetic Hsp90 drug inhibitors AUY922 and HSP990 demonstrate anti-cancer properties (restricting cell growth and promoting cell death) in prostate cell lines and primary tumours. These drugs show a higher potency than 17-AAG.
Relevance:
In Australia, prostate cancer is one of the most common types of cancer in men. Developing new therapies is a key focus of research in this area.
It has been recognised that inhibiting Hsp90 could halt the progression of prostate cancer. By understanding how this protein works at a cellular level, it has given a framework for drug development.
While drugs could be designed to achieve Hsp90 inhibition, a question always remains over which one will be more effective. Previous trials of Hsp90 inhibitors (eg. 17-AAG) have not succeeded in clinical trials due to issues with drug performance and liver toxicity.
This study highlights an ex-vivo technique that gives more insight into the potency of other Hsp90 inhibitors in human tissue. It shows a new way that drugs could be evaluated and optimally chosen for human usage.
HRA Comment
Drugs are often tested on animals to understand their effects and suitability for human use. A big drawback of this approach are the clear biological differences between animals and humans. Just because a drug delivers good results in an animal model does not mean it will function the same in human cells/tissue. This study represents a better way that pharmaceutical agents could be selected for humans instead of by trial and error in animals.
Although this study does not directly use any animals it was noted that serum and antibodies with animal hosts were utilised